GASTRIC
BANDING
If you are considering surgical options to address obesity-related health issues, we invite you to explore adjustable gastric banding at Minimally Invasive and Bariatric Surgery (MIB). Gastric banding, known as lap band surgery, is a preferred choice for many people seeking a minimally invasive option for weight loss, noted for its lower risk of complications and minimal postoperative maintenance.
How does sleeve gastrectomy work?
The gastric band, also known as an adjustable gastric band, is a medical device used in bariatric surgery to aid in weight loss. Its operation is based on the following steps:
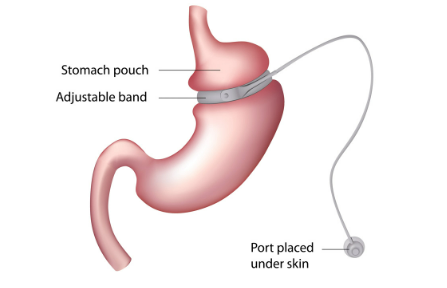
Band placement:
during laparoscopic surgery, an adjustable band is placed around the upper part of the stomach. This band is a silicone band that forms a small pouch at the top of the stomach. The pouch created has a narrow opening that connects to the rest of the stomach.
Band adjustments:
After surgery, adjustments can be made to the gastric band. This is accomplished by inflating or deflating a chamber inside the band. Adjustments are made by injecting saline solution into a subcutaneous port that is placed under the skin. These adjustments control the amount of food that can pass through the band into the main stomach.
Reduced stomach capacity: The adjustable band decreases the capacity of the upper stomach, which makes the person feel satisfied with a smaller amount of food. This limits food intake and ultimately contributes to weight loss.
Eating smaller portions: To maintain weight loss, patients must learn to eat smaller portions and select healthy foods. Overeating or high-calorie foods can lead to discomfort and vomiting.
Do I qualify for a sleeve gastrectomy?
If you answer "yes" to all of the questions below, you may qualify!
- Are you between the ages of 18 and 70?
- Do you have a BMI of 40 or more, or a BMI of 35 or more and obesity comorbidities?
- Have you been obese for 1 or more years?
- Have you tried to lose weight with non-surgical methods without success?
- Do you understand the risks, side effects and complications?
- Do you agree to make the necessary lifestyle changes?
- Can you commit to a healthy and active lifestyle?
Am I a good candidate for a gastric band?
Generally speaking, patients with a body mass index (BMI) of at least 40 are suitable candidates for gastric banding. For some people, excess weight may prevent them from qualifying for gastric bypass surgery, so gastric banding surgery may be a viable alternative.
Advantages of sleeve gastrectomy
There are many potential benefits of sleeve gastrectomy, including:
- Reduced hunger
- Shorter hospital stays and quicker recovery because it is minimally invasive compared to other bariatric surgeries
- The intestines are not bypassed
- Once the procedure is completed, no regular adjustments are needed.
- Facilitates safe weight loss
- Digestion occurs naturally
- No implantation of a medical device
- No periodic adjustment as with gastric bands
Disadvantages of sleeve gastrectomy
Sleeve gastrectomy is irreversible and, like any other surgical procedure, carries the risk of complications. These include infection, blood clots, pneumonia, postoperative pain and loss of stomach contents. Fortunately, the risk of complications is very low, making it one of the safest surgical procedures.
Before the procedure
Follow the two-week preoperative diet as prescribed. Do not eat or drink anything, including water, after midnight prior to surgery. You will be given prescriptions for medications that you will have available at home for your aftercare.
Day of the procedure
Check in pre-operatively and then your nurse and anesthesiologist will meet with you. You will be given a hospital gown to wear and asked to remove any accessories, such as watches and earrings. You will be asked to confirm your consent to the procedure. You will receive medication to help you relax and an intravenous line. Your nurse will take you to the operating room where the procedure will be performed.
Day of the procedure
You will be in the recovery unit when you wake up. Shortly thereafter, your family will be invited to visit. When our medical staff gives you the go-ahead, you will be taken to your room.
Some patients are able to leave the hospital the same day of surgery; others need one to three days of recovery in the hospital. You and your doctor will decide what is best for you.
You will receive discharge instructions and a post-operative manual, but here is a preview of post-operative guidelines:
- Drink fluids to avoid dehydration.
- Don't hesitate to ask your surgeon or nurse about any problems you experience.
- Constipation and difficult or painful bowl movements are common in the first week after surgery.
- Take your medications as recommended.
- Due to the reduced caloric intake, you will feel fatigued for approximately 2-3 weeks after surgery. This is normal. Your body is adjusting.
- Take walks. It is important to stay active for recovery, but do not overexert yourself.
- You may shower after surgery, but avoid baths and hot tubs for three weeks after surgery.
- Depending on your profession, you can return to work in approximately two to four weeks after surgery. Most patients opt to return to work in four to six weeks when their strength returns.